Pain Medicine Clinic at The Wellington Hospital
The Wellington Hospital , Wellington Place , London, NW8 9LEDon't suffer in silence
Common pain conditions we treat in our clinic
-
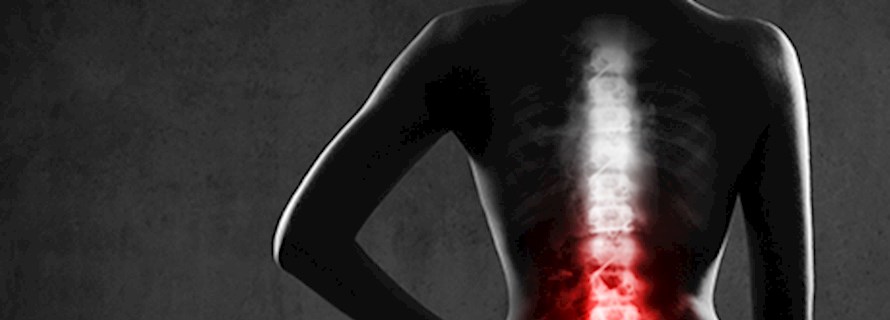
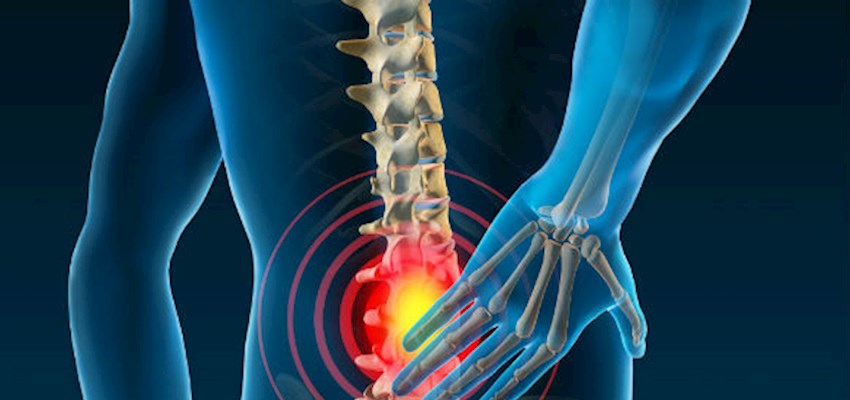
Back pain
-
Neck pain
-
Sciatica
-
Trapped nerves
-
Nerve pain
-
Cancer pain
-
Cancer-induced bone pain (CIBP)
-
Fibromyalgia
-
Headaches
-
Complex Regional Pain Syndrome (CRPS)
-
Disc herniation (inc. disc bulge, ruptured disc, slipped disc)
-
Spinal stenosis
-
Brachalgia (shoulder pain)
-
Musculoskeletal pain
-
Trigeminal neuralgia (facial pain)
-
Occipital neuralgia
-
Spondylosis
The UKs leading pain medicine specialists
They offer cutting edge treatments including spinal cord stimulation, tumour ablation, neurolytic procedures, as well as precision-guided spinal injections. They also work closely with consultants in other specialities to ensure holistic, multi-disciplinary care, and allied health professionals such as specialist psychologists and physiotherapists.
Most people get back or neck pain at some stage of their lives. Many have a number of episodes as well as sciatica or a trapped nerve in their neck. However, 95% of people with back pain don't need surgery. Our specialists will fully assess you and do all the investigations necessary, and if you need surgery you will be referred on to one of our expert partner surgeons, who will be just right for your particular problem.
Diagnosing the problem using the latest technology
If your pain is not responding to traditional painkillers, it’s likely they are no longer providing an appropriate means of managing your pain or are perhaps causing possible side effects.
When you meet our pain medicine specialists we provide a full assessment that will include imaging tests and scans, including MRI, CT, X-ray, SPECT-CT, Ultrasound, Nerve Conduction Studies and Neurophysiology to understand better the pain medicine solution that is right for you.
We do all the necessary assessments and should you require surgery we can make a quick referral for you to many of the best surgeons in the country for your specific condition.




Providing end to end pain management
We provide make a full clinical assessment, tests, imaging, physiotherapy, non-surgical treatment, pain medicine, surgery if needed and rehabilitation.
Conditions and treatment options
-
Lower back pain
Need to know
Low back pain (LBP) is a very common symptom that affects all age groups from the young to the elderly. It is one of the leading causes of disability. In most people with LBP a specific cause may never be found whilst in a minority there will be actual pathology which causes symptoms. Most cases of LBP...
-
Neck pain
Need to know
Neck pain is rarely a sign of anything serious. It can happen if you've strained a muscle or sat or slept in an awkward position. Bad posture, anxiety and stress can also lead to neck pain. Normally, the problem will go away after a few days or weeks. If yours doesn't, our spinal, neurological and orthopaedic...
-
Caudal epidural for sciatica
Need to know
A caudal epidural is an injection at the base of the spine which may help relieve the symptoms of sciatica caused by the sciatic nerve. The sciatic nerve runs from your hip to your feet. The irritation of this nerve, most commonly caused by a slipped disc but also by a narrowing or misalignment of the...
-
Spinal stenosis
Need to know
In response to the ageing process, wear and tear, or an inherited predisposition, your spinal canal can become too narrow, compressing the nerves inside. This is known as spinal stenosis. When it occurs in the lumbar spine it may or may not be associated with leg pain. In the neck the pressure is on...
-
Slipped disc
Need to know
A herniated or 'slipped' disc is when one of the discs separating our vetebrae ruptures. This happens when the disc starts to degenerate, causing the disc to bulge backwards and even split. This can press on the spinal cord or nerves, causing pain. This has in the past been described as ‘Sciatica’ when...
-
Epidural for pain management
Need to know
During a caudal epidural, an anti-inflammatory medicine, such as hydrocortisone, is injected round the areas of inflammation in the spinal canal. This injection is used when nerves in the lower back are inflamed due to irritation from either spinal stenosis (a degenerative narrowing of the spinal...
-
Sacral nerve root injection
Need to know
The sacral nerve is part of the sacral plexus, a network of nerve fibres that supply the skin and muscles of the pelvis and lower limb. The network is located on the surface of the posterior pelvic wall and the anterior to the piriformis muscle. If you have persistent back, hip or limb pain, your...
-
Sacral nerve stimulation
Need to know
By stimulating the relevant nerves in your lower back with mild electrical impulses, a neurostimulator device can improve the co-ordination between your brain and your bladder, bowels, pelvic floor and sphincter muscles. Your consultant may recommend this if other treatments haven't worked.
-
Facet joint injection
Need to know
Facet joints are thumbnail-sized pairs of joints in the neck, mid and lower back. Sometimes, they can cause pain in the head, neck, shoulders, chest, abdomen, bottom, groin or legs. A time-release steroid injection can be used to locate which joints are causing pain and help reduce inflammation.
-
Nerve pain
Need to know
Nerves branch out from the spinal cord to other parts of your body. These enable messages to travel from your brain to other parts of your body; it's down to this that we're able to run and walk. The nerves in your back carry messages about sensations and muscle controls to your brain. When these nerves...
-
Facial pain
Need to know
Facial pain can occur even when the structures of your mouth, jaw and face are healthy. In chronic facial pain, there is a disturbance in the transmission of pain messages to your brain. Nerves carrying the pain signals have a memory for transmitting pain. These nerves become extremely sensitive and...
-
Knee pain
Need to know
If you have pain, discomfort, swelling or restricted movement in your knee, it can affect every aspect of your day-to-day life. These problems may result from an injury or wear and tear that gets worse over time. Our knee specialists are here to help diagnose a wide range of injuries and conditions,...
-
Wrist pain
Need to know
Any pain, discomfort or restricted movement in your wrist can have a major impact on day-to-day life. This may be the result of an injury, such as a fall, or wear and tear that worsens over time. Our hand and wrist specialists are here to help diagnose a wide range of injuries and conditions, and offer...
-
Neuropathic pain
Need to know
If you have neuropathic pain you may experience burning, aching or electric shock sensations in the parts of the body supplied by the affected nerve. You may also experience pins and needles, numbness and weakness. Unlike most types of pain, neuropathic is usually unresponsive to common painkillers.
-
Peripheral neuropathy
Need to know
The peripheral nervous system is a network of nerves in your body. It controls your hands, feet and arms. Sometimes, these nerves can be damaged, leading to pain, weakness and numbness. This condition is known as peripheral nephropathy. It affects 1 in 10 people over the age of 55. If you're experiencing...
-
Nerve conduction studies
Need to know
Nerve conduction studies help measure the speed at which nerves send messages to the brain. This is done by placing electrodes on your skin. Your consultant then uses electrical activity to record how fast impulse moves along a nerve. The tests normally lasts no longer than one hour.
-
Dorsal root ganglion stimulation
Need to know
Pain impulses are conducted by fine nerve fibres entering the back of the spinal cord at each vertebral level. With spinal stimulation, an implanted electrode stimulates the dorsal columns (nerve fibre bundles at the back of the spinal cord), to impair the transmission of the pain fibres and reduce or...
-
Nerve compression
Need to know
Nerve compression syndrome (trapped nerves) can cause pain and loss of nerve function. They are usually caused by chronic compression. Compressed nerves often happen in the arm, around the elbow (cubital tunnel syndrome) and the wrist (carpal tunnel syndrome). More rarely, they can occur in the lower...
-
Brachialgia
Need to know
Brachialgia, or cervical radiculopathy, describes pain in the arm caused by a pinched nerve in the neck.
-
Chronic pain
Need to know
Chronic pain is when pain lasts for a significant length of time, beyond three months. There can be many reasons for the pain, including nerve damage or pain following an accident or operation. It can also be a result of a condition such as arthritis or multiple sclerosis.
-
Trigeminal neuralgia
Need to know
Trigeminal neuralgia is a severe and sudden type of facial pain. It's believed to be caused by an artery or vein compressing your trigeminal nerve (the nerve that gives feeling to the face). These attacks can lead to anxiety as well as actual pain. To help this, we offer a range of treatment options...
-
Occipital neuralgia
Need to know
Occipital neuralgia causes intense, shock-like pain in the back of the head, as well as migraine-type symptoms. It's often caused when the occipital nerve, which travels along the neck and up to the base of the skull, becomes trapped. Routine activity such as brushing the hair or lying with your head...
-
Ankylosing spondylitis
Need to know
Ankylosing spondylitis (AS) is a long-term condition that causes inflammation in the spine and other areas. It is more common in men, and mostly begins during your teens or early adulthood. It tends to develop gradually and symptoms, including a stiff or painful back, may come and go. It's not known...
-
Sacroiliac joint pain
Need to know
The sacroiliac joint or SI joint is the joint between the sacrum and the ilium bones of the pelvis linking the lower spine and the pelvis. When the sacroiliac joints at the base of your spine stop working properly, it can sometimes cause lower back and leg pain. The pain can present similar symptoms...
Radio frequency treatment for back pain and neck pain
We can put a probe into your back and send a radiofrequency signal through the probe to destroy damaged nerves, and prevent signals being sent through the spinal cord to your brain, thereby relieving your pain.
Image guide injections
A corticosteroid (steroid) injection, guided by ultrasound, can be an effective way to treat spinal, joint or nerve problems. Corticosteroid injections are most often used to treat joint inflammation (synovitis), which may occur in the back, shoulder, knee and hip. They may also be used to treat inflammation around tendons and ligaments.
The injection is usually a combination of anti-inflammatory steroid and local anaesthetic, with the needle being carefully guided by ultrasound.

Spinal cord stimulation
Spinal cord stimulation (SCS), often called neuromodulation or dorsal column stimulation, is a specialist technique used for a range of spinal and nerve problems. Pain impulses are conducted by fine nerve fibres entering the back of the spinal cord at each vertebral level. With spinal stimulation, an implanted electrode stimulates the dorsal columns (nerve fibre bundles at the back of the spinal cord), to impair the transmission of the pain fibres and therefore reduce or eliminate the pain.
SCS can be a successful technique in treating severe disabling pain, nerve injury or after spinal surgery, such as Failed Back Surgery Syndrome (FBSS) and Complex Regional Pain Syndrome (CRPS). In our Pain Medicine Clinic we perform more SCS procedures each year than any other private hospital, providing patients with pain relief when most other pain management options have failed.


Tumour ablation treatment
We frequently help patient who have benign and metastatic bone tumours which have not proven responsive to radiotherapy with a treatment called tumour ablation. CT-guided laser energy destroy the tumour whilst leaving the surrounding healthy tissue undamaged.
Complex spinal care

Our peripheral nerve injury unit
Our specialist peripheral nerve injury unit, led by consultant Mr Marco Sinisi, specialises in every aspect of peripheral nerve injury and we can facilitate a quick referral to the unit within The Wellington Hospital should you need it.
Whether you're experiencing pain from a previous nerve injury, have lost sensation, or you've experienced a traumatic injury to a nerve, they offer you the highest level of care.


Our spinal unit
We treat all forms of spinal conditions, from chronic back pain to scoliosis, and everything in between including spinal tumours, spinal injuries, disc prolapse and slipped discs.
Under our care, you'll benefit from the expertise of a multidisciplinary team, including our leading spinal surgeons, radiologists, oncologists and anaesthetists, as well as spinal clinical nurse specialists.

Pain and the performing arts
What help is there for performers who are in pain?
What kind of health problems do performers experience?




Contact the Pain Medicine Clinic
We can offer same-day appointments with a Pain Medicine consultant. If you would like to make an appointment please contact us, we’ll be happy to help.
Call us on
020 7483 5148